A Nipah virus (NiV) outbreak in northern Bangladesh has caused widespread panic throughout the country, with many residents deserting their homes for fear of contacting the virulent disease. The pathogen has infected a total of 30 patients since early 2011. All of the patients known to have contracted the virus have died. Professor Mahmudur Rahman, director of the Institute of Epidemiology, Disease Control and Research (IEDCR) in Dhaka says, “In the last two years, the mortality rate has been 100 percent. Once the disease sets in, nothing much can be done.”
Bangladesh has experienced continuous outbreaks of Nipah virus since 2001, when it was first discovered as an ‘unknown’ ailment. Finally in 2004, after another 50 deaths in Bangladesh went unexplained, a U.S. lab detected Nipah virus as the causative agent. Currently, Bangladesh is the only country reporting the disease. However, the virus has plagued various Asian countries over the past couple decades, in particular Malaysia, Singapore, and India.
First Outbreak of Nipah virus
In 1997, a combination of deforestation, drought, and wildfires caused flying foxes (large fruit bats now known to be the reservoir for NiV) to migrate from their natural rainforest habitat to seek nourishment and shelter in fruit orchards surrounding pig-farms. It is believed that pigs contracted the virus by scavenging fruit contaminated with bat urine and saliva. The virus spread rapidly and viciously from pig-to-pig and from there to farm workers who had been in close contact with the pigs. Unfortunately, Malaysian pig farmers sold their livestock across the Asian continent, and by early 1999 the first cases of Nipah virus appeared in Singapore. Finally in March of that same year the virus was identified, allowing public health authorities to initiate rigorous control methods to impede the spread of the disease, such as banning the import of pigs from Malaysia, closing slaughterhouses, and culling over one million pigs. While these procedures helped control the virus, approximately 40 percent of patients infected with the disease had already died. Additionally, the outbreak almost destroyed the pig-farming industry in Malaysia. The government suffered a loss of approximately $450 million.
Pathway of Transmission
There are three known pathways of transmission of NiV from bats to people. In Bangladesh, a majority of people infected with the pathogen became infected from contaminated fresh date palm sap. Drinking the sap in the morning is a common cultural practice in the rural areas of Bangladesh. It is recommended to boil the sap before consumption, since the virus is killed at 70 degrees Celsius.
The initial outbreak in Malaysia was characterized by the second mode of transmission: via domestic animals. Pigs are viable intermediate hosts, however reports of infected cows, goats, and even dogs have also surfaced.
Last, direct contact with NiV-contaminated fruit bat secretions can cause infection in humans. This was seen in cases in Goalando, Bangladesh, where persons climbed trees and were consequently infected with the virus.
Bangladesh has had the highest number of NiV cases transmitted by person-to-person contact with a sick individual. Respiratory secretions are particularly important, as the virus has been detected in patients’ saliva. Social norms in Bangladesh play an important role in the spread of the disease between people. It is expected that close family members care for their sick. In many cases, care providers continued to share utensils and glasses with the sick patients, sleep in the same bed, and even provide close physical contact such as hugging and kissing. In one example, an infected religious leader transmitted the Nipah virus to 22 of his caretakers.
Environmental Considerations
Nipah virus is only one of many zoonotic infections considered to be emerging pathogens. In fact, over the last century more than 75 percent of emerging infectious diseases (EID’s) were from zoonoses. The increasing number of animal-to-human diseases can be at least partially attributed to human environmental mismanagement.
When the Nipah virus was first discovered in Malaysia, approximately 5 million hectares of tropical rainforest had been cleared to allow room for the growing number of piggeries. Additionally, the slash and burn agriculture used to raze the forest created a blanket of haze over the region. The combination of all these factors destroyed a significant number of the flowering and fruit trees which the flying foxes required for survival. Deforestation leads to the encroachment of the bats into human habitats and is directly linked with the spread of NiV.
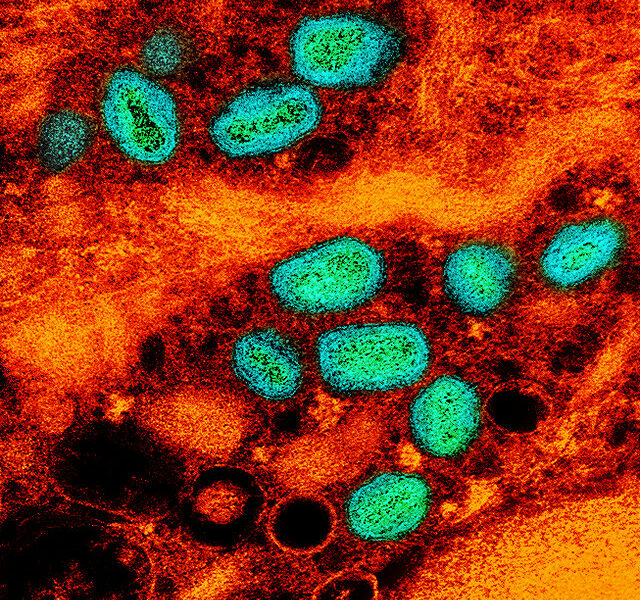
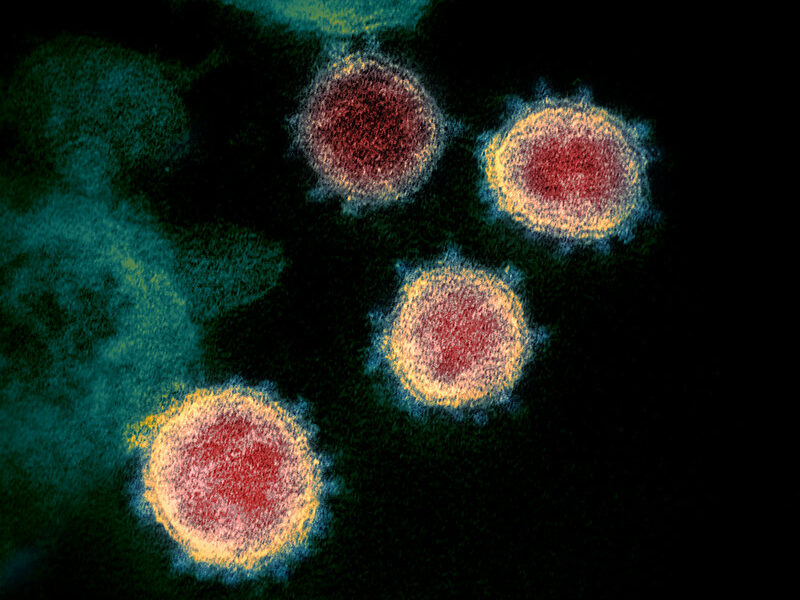
Infection with Nipah virus
Nipah virus manifests itself in a variety of ways, ranging from asymptomatic infection to severe encephalitis. Initial symptoms are similar to influenza and include: fever, headaches, myalgia, vomiting, and sore throat. Drowsiness, dizziness, and altered consciousness may follow, as well as neurological signs that are indicative of encephalitis (inflammation of the brain). Some patients also experience respiratory illness, such as pneumonia and acute respiratory distress, and seizures. Within 24 to 48 hours, patients progress to a coma and then death. Around 20 percent of patients who survive acute encephalitis suffer from residual neurological damage. The case fatality rate of infection with NiV ranges from an average of 40 to 75 percent, however this can vary significantly per outbreak.
Although there is no treatment or cure for NiV infection, there are a number of prevention strategies that greatly minimize the risk of contacting the virus. It is essential that individuals either stop drinking fresh date palm sap entirely or boil it to kill the virus. Additionally, family members should minimize exposure with ill patients and healthcare providers should wash their hands frequently and use personal protective equipment. Last, it is essential that communities practice improved forest management techniques to maintain the natural habitat of the flying foxes.