By: Jessica Wise and Autumn Gertz
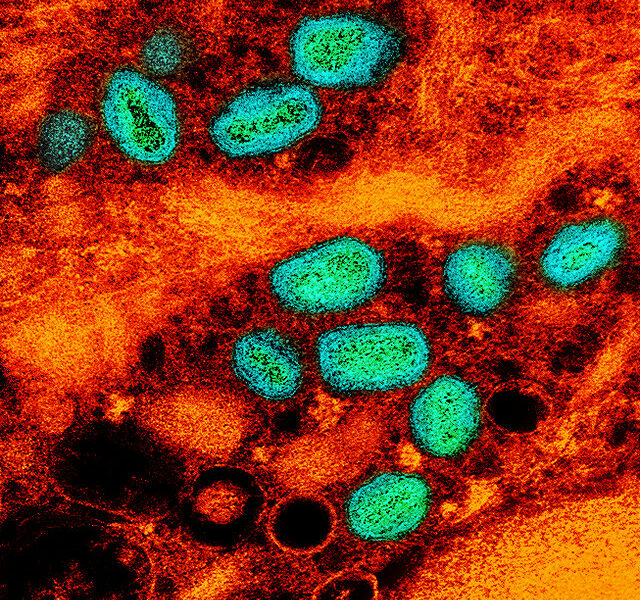
Tuberculosis (TB) is an infectious disease similar to COVID-19: both respiratory illnesses are spread from person-to-person via droplet transmission [1]. Contrary to the massive influx of COVID-19 cases in early 2020, the number of TB cases worldwide was at its all-time low [2]. However, the COVID-19 pandemic has increased the global burden of TB due to delays in diagnostic testing and treatment [2].
Tuberculosis is considered a disease of poverty such that poverty fuels TB transmission. Major drivers of TB transmission include the absence of robust healthcare services, poor nutrition, and inadequate living conditions [3]. Countries in Africa, Asia, and Latin America are where TB is most prevalent, with India being the country with the highest number of TB cases each year [3]. India is responsible for over twenty percent of the world’s TB cases, and the pandemic has caused a 75% reduction in TB diagnoses [2].
The primary problems affecting TB diagnosis and treatment that resulted from the COVID-19 pandemic are lockdowns and travel restrictions. Since TB is commonly found in low-income countries, many patients must travel far distances to seek TB diagnosis and treatment, and the ability to do so has been hindered by lockdowns and travel restrictions [2]. Additionally, TB spreads most efficiently when humans are in close contact indoors, which is also a concern for household transmission for those quarantining together [2]. International travel restrictions are affecting supply chain distributions as diagnostic tests and medications to treat TB are not being delivered as frequently, ultimately leading to delays in diagnosis and treatment [2]. With a rise in the number of undiagnosed TB cases in 2020, we can expect a massive increase in the number of TB cases next year [2].
Another major area of concern that results from interruptions in supply chain is medication shortage, which forces patients to ration their medication or stop treatment [2]. TB treatment requires patients to take several drugs for anywhere from six to nine months, and TB patients who stop using their medication too soon can get sicker [1]. Also, misusing TB medication can cause TB bacteria to become resistant, and drug resistant TB is much more difficult to treat. [1; 4].
Ultimately, there is a threat of a rise in TB infections globally in the upcoming years as nations continue to allocate their resources to the COVID-19 pandemic. Healthcare systems need to strengthen their ability to care for TB patients or those at risk of TB infection.
References
[1] https://www.cdc.gov/tb/topic/treatment/tbdisease.htm
[2] https://www.nytimes.com/2020/08/03/health/coronavirus-tuberculosis-aids-…
[3] https://www.who.int/news-room/fact-sheets/detail/tuberculosis
[4] https://www.sciencedaily.com/releases/2020/06/200624103257.htm