Image courtesy of United Nations Photo via Flickr Creative Commons
The World Health Organization (WHO) identified nine new polio cases caused by the polio vaccine in Nigeria, Congo, Central African Republic and Angola in November. The total number of children this year affected by vaccine-derived polio infections in the world has risen to 177 through December 2019, while the wildtype poliovirus has affected 112 children globally [1]. Vaccine-derived polio is caused by a mutated strain of the polio vaccine [2]. It is more prevalent in non-endemic countries like those in Africa, while all wildtype polio have only occurred in endemic countries like Afghanistan and Pakistan [1]. The increasing vaccine-derived polio cases raise concerns that although many countries made achievement in preventing and eradicating wildtype polio, the vaccine-derived polio brings increased threat and a new mutation strain could occur in the future.
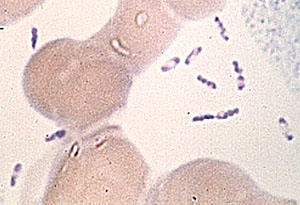
Polio is a highly infectious viral disease caused by the poliovirus [3]. The disease is very contagious and spreads from person to person through contact with the feces of an infected person. It is also transmitted through droplets from a sneeze or cough of an infected person [4]. The disease mainly affects young children under five years of age, causing paralysis by invading the infected person’s brain and spinal cord. The symptoms usually start as sore throat, fever and nausea and become severe including paresthesia, meningitis and paralysis [4]. Polio cannot be cured, but it can be prevented through effective immunization. There are two types of vaccine that can prevent polio: inactivated poliovirus vaccine (IPV) and oral poliovirus vaccine (OPV). Only IPV has been used in the United States since 2000; however, OPV is still used throughout much of the world [4].
There are three wild types of poliovirus: type 1, type 2 and type 3 [5]. After type 2 poliovirus was declared eradicated in 2015, the world switched trivalent OPV, which targets 3 type poliovirus, to bivalent OPV, which targets type 1 and type 3. However, vaccine-derived poliovirus was mutated from the components of attenuated type 2 virus containing in trivalent OPV before. The current bivalent OPV is less effective in vaccine-derived polio cases. The weakened poliovirus in OPV also has the potential to mutate over time resulting in the outbreak of new vaccine-derived poliovirus in the future [3]. IPV is more effective than OPV because it can target type 1, type 3 and vaccine-derived polio. It does not contain live virus and has less risk of mutation. Centers for Disease Control and Prevention of the U.S. suggest that after eradicating all wildtype polio, it is important to shift to IPV from OPV to eliminate the risk of vaccine-derived poliovirus [4].
The recent vaccine-derived polio outbreak in Africa was caused by low vaccination rates [6]. The virus was found in fecal matter and spread to children who have not been vaccinated. To eradicate polio, more than 95% of a population needs to be immunized. WHO and partners have long relied on OPV because it is inexpensive and can be easily administered, requiring only two drops per dose. Vaccine-derived polio outbreaks in the past were rapidly stopped by multiple rounds of high-quality immunization campaigns. Therefore, the solution by WHO for current outbreak still focuses on immunization for every child several times with the OPV to stop disease transmission [2].
References
[1] http://polioeradication.org/polio-today/polio-now/this-week/
[2] https://www.who.int/features/qa/64/en/
[4] https://www.cdc.gov/polio/about/index.htm
[5] https://www.cdc.gov/cpr/polioviruscontainment/diseaseandvirus.htm