By: Jiayan Liu
Image courtesy of Food Group via Flickr Creative Commons
Situation in New Jersey:
The New Jersey Department of Health reported on November 4th that a deli worker at the ShopRite in Somerville, New Jersey was infected with hepatitis A and worked during a time when the virus could have been spread to others [1]. The food handler worked from Oct 13th to 30th when he or she was infectious. Officials recommended that any items purchased from the in-store deli at ShopRite of Somerville from Oct 13th to 30th should be thrown away. People who ate items purchased at the ShopRite and did not get hepatitis A vaccine previously should get the vaccine within two weeks to prevent getting sick. Health officials also conducted three hepatitis A vaccination clinics and offered free vaccines on Nov 6th and 7th. New Jersey’s current hepatitis A outbreak began in 2018, and there have been 512 confirmed cases as of early November [2]. Six deaths were confirmed, and 337 confirmed cases have resulted in hospitalizations.
What is Hepatitis A?
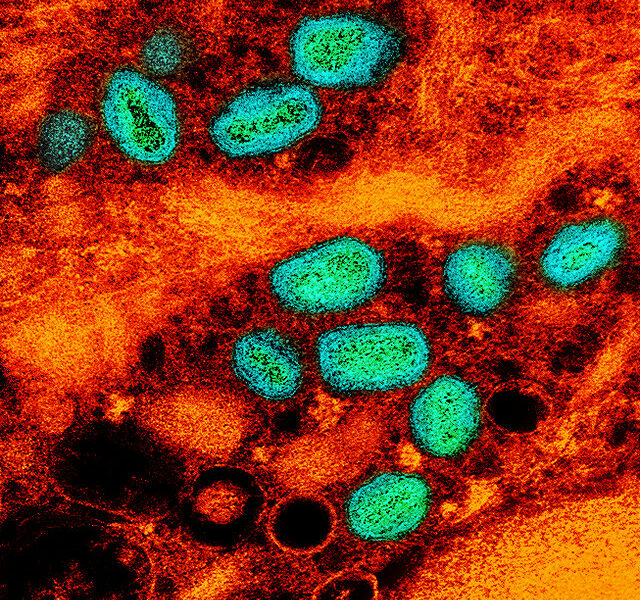
Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus [3]. It is usually transmitted person-to-person through the fecal-oral route of consumption of contaminated food or water [3]. Hepatitis A is a self-limited disease that does not result in chronic infection. The majority of infections occur among people who are experiencing homelessness, intravenous drug users, and men who have sex with men [3]. Symptoms of the disease include fatigue, low appetite, stomach pain, nausea, vomiting and jaundice. There is no specific treatment other than rest, adequate nutrition, and fluids. The best way to prevent hepatitis A infection is to keep hand hygiene and to be vaccinated. The vaccine is highly effective and has long-term protection [3].
Ongoing Outbreak in the USA:
The hepatitis A outbreak in New Jersey is part of the ongoing nationwide outbreak of hepatitis A infection, which began in 2016 and has led to 28,111 cases in the US [3]. The outbreak was started by the imported food in California and Michigan and subsequently hit 29 states. Health officials assumed that the current outbreak of hepatitis A is related to the opioid epidemic and drug use [4]. Past cases were often caused by contaminated food and scaled up by transmission among drug users and homeless individuals. Many hepatitis A cases are concentrated in states with high opioid overdose rates, including Ohio, Tennessee and West Virginia. Due to its means of transmission, hepatitis A spreads quickly through communities of people where sanitation is not available or not emphasized. Homeless and prison populations are ideal for the infection to thrive, and often, areas heavily impacted by the opioid epidemic have larger percentages of people experiencing homelessness. Government outreach programs have begun trying to combat the spread of the infection in these populations to slow its growth across the US. While extenuating circumstances, like homelessness, increase the spread, anyone who is unvaccinated can be infected with hepatitis A if exposed.
References
[1]https://patch.com/new-jersey/bridgewater/somerville-shoprite-deli-worker-was-infected-hepatitis
[3]https://www.cdc.gov/hepatitis/hav/index.htm
[4] https://www.addictioncenter.com/news/2019/08/hepatitis-a-opioid-epidemic/