On December 14th, the Centers for Disease Control and Prevention (CDC) designated Brownsville, Texas as a Zika cautionary zone after the Governor Greg Abbott reported confirmed cases of local transmission [1, 2]. Texas’ first locally transmitted case of Zika was announced on November 28 and five more cases have been identified since. Five of the cases live very close to the index case and developed Zika-like symptoms several days before mosquito control efforts went underway [3]. On December 22, the Department of State Health Services (DSHS) announced that a sixth case was identified and does not appear to be connected with the other cases [4]. This is the second state in the US to have reported local transmission of Zika virus, a mosquito-borne and sexually transmitted virus, widely feared because of the devastating teratogenic effects it can cause, including – but not limited to – microcephaly.
Brownsville, Texas is the county seat of Cameron County and is situated on the southeastern tip of the Texas-Mexico border. South of Brownsville, across the Rio Grande River, is the Mexican city of Matamoros. Travel across the border is common between the two cities. The Mexican Tourism Board has been reporting mosquito transmission of Zika on their side of the border at least since April 15, 2016, and it is possible that the virus has been circulating in Matamoros [5]. Approximately six months earlier, the DSHSof Texas announced the first local transmission of chikungunya in Cameron County and have also reported local transmission of dengue in previous years [6, 7]. It may only be a matter of time before Zika joined these other arborviruses in spreading to Texas.
Zika Symptoms and Birth Defects
The symptoms of Zika virus infection are generally mild and commonly include a fever, rash, joint pain, and/or conjunctivitis. However, it should be noted that most people exhibit no symptoms at all [8, 9]. Asymptomatic cases are a cause of concern because these individuals may unknowingly spread the disease to their sexual partners or to uninfected mosquitoes, which may end up transmitting the virus to other humans. Infected pregnant women are largely at risk as the virus has been associated with microcephaly in infants infected in utero, but it is not fully understood when pregnant women are at the greatest risk. Two new studies further illuminate the dangers of the Zika virus in child-bearing women. Both studies reported that infection during the first trimester had the greatest chance of yielding adverse outcomes for the fetus [9, 10]. One study of symptomatic and asymptomatic women registered with the US Zika Pregnancy Registry showed that 6% of the babies born from the study population had birth defects, with the majority of them being microcephaly (18 births out of 26 total births with defects) [9]. Other abnormalities were also seen in infected infants, both with and without microcephaly. These widely differing teratogenic effects included neural tube defects, congenital contractures, deafness, intraocular calcifications, and many other brain or eye abnormalities [9]. A second study in Brazil of symptomatic pregnant women only demonstrated unsettling results in that 46% of the children born from these women had birth defects but only four of the these 58 children had microcephaly [10]. Some of these Brazilian women were co-infected with other diseases, such as chikungunya or syphilis, and many of them had previous dengue infections [10]. The large discrepancy of the amount of birth defects may be due to an unknown condition that exists between the two study populations. Differences in the populations include previous dengue infections, geography, and the possible inclusion of false positive women in one of the studies [11]. Regardless of the real risk of Zika related birth defects, it is highly recommended that pregnant women protect themselves in areas where Zika may be circulating.
Babies born without any apparent birth defects to Zika infected mothers may have or develop problems as they grow. The CDC and researchers from Brazil have reported 13 cases where children with normal head sizes had laboratory evidence of congenital Zika infection [12]. Of these children, 11 showed decreased head growth at as early as five months of age and were later diagnosed with microcephaly [12]. All of the 13 children born with normal head sizes were found to have adverse brain abnormalities, such as subcortical calcifications and motor disabilities [12]. These findings solidify the importance of early neuroimaging and follow-up exams for children exposed to the Zika virus [12].
For mothers faced with raising a child with Zika-related birth defects, one can only guess at the life-long cost of treatment and care. The director of the CDC, Dr. Tom Frieden, estimated in a press conference in April that a single child with birth defects can cost over $10 million USD [13]. Barbara Altman, a woman who has a 53 year old microcephalic son, estimates Medicaid payments for the care of her child costs $395,600 a year and over $21 million dollars over his lifetime so far [14]. As of November 30th, there have been at least 32 children born with Zika-related birth defects in the US alone [15], which may cost families and taxpayers over $12.5 million dollars a year using Ms. Altman’s estimate.
Controlling Zika
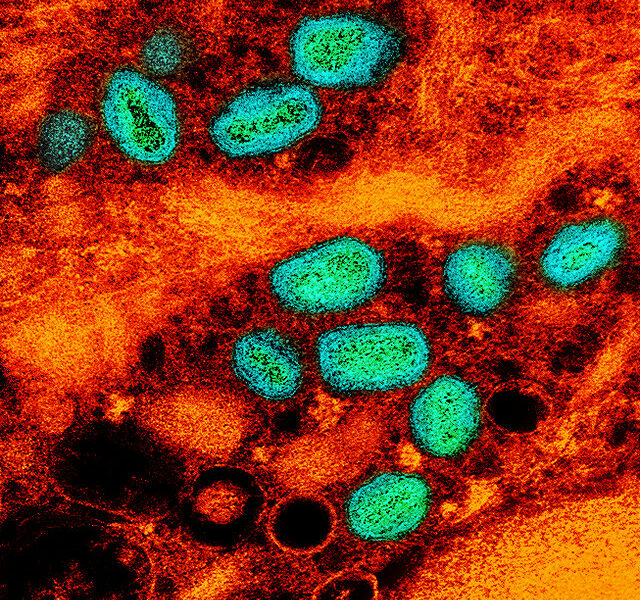
The principle vector of the Zika virus, the Aedes aegypti mosquito, is estimated to be present in roughly half of the contiguous United States [16]. It is imperative to keep these local mosquitoes from becoming infected with the virus as this will prevent local transmission. Many varied public health interventions to control mosquito populations have been used for decades, but evaluating their effectiveness has proven inconclusive [17]. A meta-review published on December 7th compared studies that reviewed biological, chemical, educational, and integrated (any combination of the previous three) vector control strategies for Aedes mosquitoes [17]. The study showed that biological control and educational programs reduced mosquito populations and breeding habitats respectively, but integrated control strategies had mixed results [17]. Chemical control may not be able to sustainably reduce mosquito populations over time and may be associated with a false sense of security that leads to decreased community involvement [17].
Due to the uncertain effectiveness of mosquito control strategies, it cannot be stressed enough that the population should take steps to reduce the risk of contracting the Zika virus and make changes to their homes and backyards to prevent Aedes mosquitoes from reproducing. Aedes mosquitoes are aggressive biters that are highly adapted to peridomestic environments and prefer human hosts [17, 18]. Once a week, any items that may contain standing water, such as tires or flowerpots, should be turned over to remove the water where mosquitoes may lay their eggs [19]. Indoor and outdoor insecticides can be used to treat areas where mosquitoes may rest while insect repellants can be used when people go outside in areas where Zika is circulating [3, 19].
Since January 2015, at least 4,757 Americans have been infected, and at least 216 of these cases getting the virus from local mosquitoes [20]. All but six of these local transmissions were in Florida, where efforts to break the transmission cycle have been ongoing since the first local cases were discovered in July [21]. An infected person importing the virus is the most common way Zika circulates into new areas [22]. Travelers coming back from areas where Zika is present should take precautions against local mosquitoes for at least three weeks [23]. Safe sex practices should also be adhered to for at least six months for men and at least eight weeks for women after travelling or developing symptoms to prevent human-to-human transmission [24]. If the local mosquito population has circulating Zika virus, widespread insecticide spraying should be undertaken to reduce the mosquito population. However, success relies on the combined efforts of the population and health authorities to prevent the spread of this disease.
Local transmission in Texas represents a new front in the fight to prevent Zika from establishing itself in the United States. Vector control efforts alone may not be enough to prevent Zika infected mosquitoes from establishing themselves into new areas. Preventing the spread of Zika must be achieved through a combined effort of health authorities and the population to keep this disastrous disease from further harming unborn children.
Sources
1. Abbott, G. State Of Texas Receives $5 Million Grant From Centers For Disease Control To Combat Zika Virus. 2016 December 12, 2016 December 15, 2016]; Available from: http://gov.texas.gov/news/press-release/22947.
2. CDC. Advice for people living in or traveling to Brownsville, Texas. 2016 December 14, 2016 December 15, 2016]; Available from: https://www.cdc.gov/zika/intheus/texas-update.html.
3. DSHS. Texas Announces Additional Local Zika Cases in Cameron County 2016 December 15, 2016 December 15, 2016]; Available from: http://dshs.texas.gov/news/releases/2016/20161209.aspx.
4. DSHS. Additional Locally-Acquired Zika Case in Cameron County. 2016 December 22, 2016 December 24, 2016]; Available from: http://dshs.texas.gov/news/releases/2016/20161222.aspx.
5. Mexico updates map of locations of Zika cases. 2016 May 3, 2016 December 20, 2016]; Available from: http://www.travelweekly.com/Mexico-Travel/Mexico-updates-map-of-locations-of-Zika-cases.
6. Coston, M. Texas DSHS Announces 1st Locally Acquired Zika Case. 2016 November 28, 2016 December 16, 2016]; Available from: http://afludiary.blogspot.com/2016/11/teas-dhsh-announces-1st-locally.html.
7. Joseph, A. Texas confirms its first case of local Zika transmission. 2016 November 28, 2016 December 16, 2016]; Available from: https://www.statnews.com/2016/11/28/texas-zika-case/.
8. CDC. Symptoms. 2016 June 28, 2016 December 16, 2016]; Available from: https://www.cdc.gov/zika/symptoms/symptoms.html.
9. Honein, M.A., et al., Birth defects among fetuses and infants of us women with evidence of possible zika virus infection during pregnancy. JAMA, 2016.
10. Brasil, P., et al., Zika Virus Infection in Pregnant Women in Rio de Janeiro. New England Journal of Medicine, 2016. 375(24): p. 2321-2334.
11. Branswell, H. With latest Zika research, our picture of the virus gets cloudier. 2016 December 16, 2016 December 20, 2016]; Available from: https://www.statnews.com/2016/12/16/zika-mess/.
12. Jenco, M. CDC: Infants with Zika can develop microcephaly later. 2016 November 23, 2016 December 16, 2016]; Available from: http://www.aappublications.org/news/2016/11/23/Zika112316.
13. CDC. Transcript for CDC Telebriefing: Zika Summit Press Conference. 2016 April 1, 2016 December 16, 2016]; Available from: https://www.cdc.gov/media/releases/2016/t0404-zika-summit.html.
14. Altman, B. The cost of caring for a child with microcephaly for 53 years. 2016 November 28, 2016 December 16, 2016]; Available from: https://www.washingtonpost.com/national/health-science/the-cost-of-caring-for-a-child-with-microcephaly-for-53-years/2016/11/22/681a2bde-a5f4-11e6-ba59-a7d93165c6d4_story.html?utm_term=.4d1357767e24.
15. CDC. Outcomes of Pregnancies with Laboratory Evidence of Possible Zika Virus Infection in the United States, 2016. 2016 December 8, 2016 December 16, 2016]; Available from: https://www.cdc.gov/zika/geo/pregnancy-outcomes.html.
16. McCandless, B. Is Zika Coming Soon To A Mosquito Near You? 2016 November 6, 2016 December 15, 2016]; Available from: http://www.cbsnews.com/news/60-minutes-overtime-zika-virus-mosquito/.
17. Bouzid, M., et al., Public Health Interventions for Aedes Control in the Time of Zikavirus– A Meta-Review on Effectiveness of Vector Control Strategies. PLOS Neglected Tropical Diseases, 2016. 10(12): p. e0005176.
18. CDC. Transmission & Risks. 2016 October 24, 2016 December 16, 2016].
19. CDC. Controlling Mosquitoes at Home. 2016 September 6, 2016 December 16, 2016]; Available from: https://www.cdc.gov/zika/prevention/controlling-mosquitoes-at-home.html.
20. CDC. Case Counts in the US. 2016 December 21, 2016 December 24, 2016]; Available from: https://www.cdc.gov/zika/geo/united-states.html.
21. Goldschmidt, D. Florida health officals confirm local Zika transmission. 2016 July 29, 2016 December 15, 2016]; Available from: http://www.cnn.com/2016/07/29/health/florida-health-officials-confirm-local-zika-transmission/.
22. CDC. Technical Statement on the Role of Disinsection of Airplanes or Ships in the Context of Zika Outbreaks, 2016. 2016 September 1, 2016 December 15, 2016]; Available from: https://www.cdc.gov/zika/vector/disinsection.html.
23. CDC. Plan for Travel. 2016 September 30, 2016 December 15, 2016]; Available from: https://www.cdc.gov/zika/prevention/plan-for-travel.html.
24. CDC. Protect Yourself During Sex. 2016 October 5, 2016 December 15, 2016]; Available from: https://www.cdc.gov/zika/prevention/protect-yourself-during-sex.html.