Although endemic in parts of Latin America, studies show that it is hard to transmit Chagas disease. Research studies have estimated that for one infected human, on average, more than 1,700 bites from the disease’s vector – triatomine bugs – are necessary for successful transmission to occur [5]. The figures are similar for the infection of guinea pigs, averaging 1,400 bites [5]. While those figures imply that transmission of the disease is fairly inefficient, for some communities in Latin America, Chagas disease infection prevalence exceeds 40% of the population [5]. A recent study published in the Proceedings of the Royal Society B suggests that guinea pigs may be the culprit for the high rates of endemicity – at least in Arequipa, Peru [5].
Overview of Chagas Disease
According to the World Health Organization (WHO), Chagas disease is endemic in 21 Latin American countries, but its geographic breadth is spreading quickly [1]. In recent years, the disease has been detected in the United States, Canada, European, and Western Pacific countries. This spread may be due to frequent international travel and population mobility from the affected countries of Latin America [1]. Approximately six to seven million people are estimated to be infected with Chagas disease, with the majority of cases happening in Latin America [1]. However, it is important to note that these numbers may be underestimated, as Chagas often goes undiagnosed due to its asymptomatic nature in humans.
Chagas: Transmission
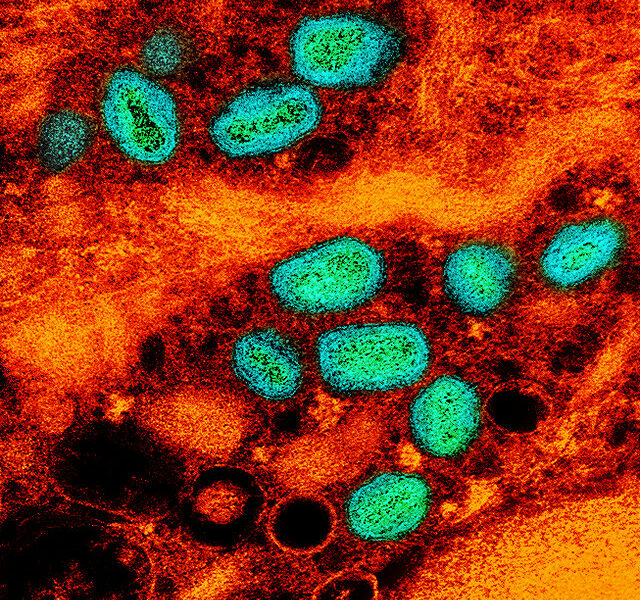
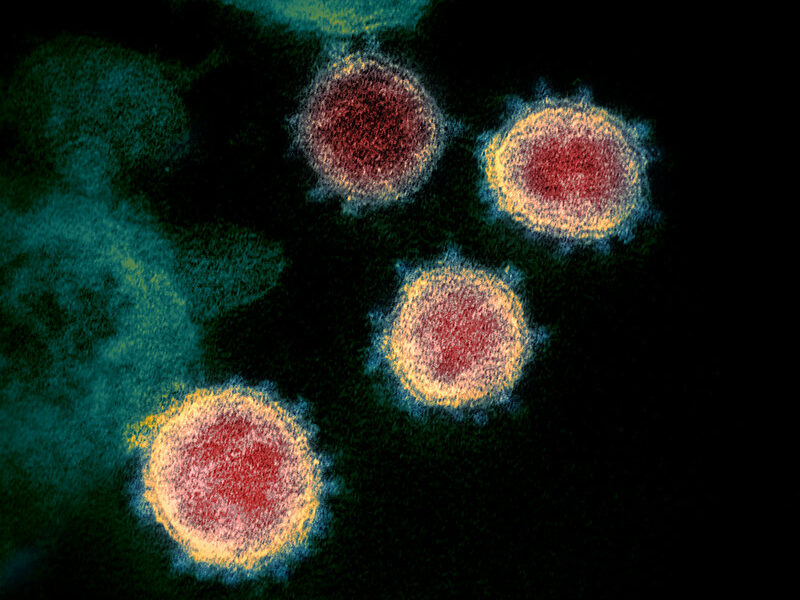
Discovered in 1909 by Brazilian doctor, Carlos Ribeiro Justiniano Chagas, the potentially life-threatening illness known as Chagas disease is caused by a protozoan parasite called Trypanosoma cruzi (T. cruzi) [1]. Chagas, also known as American trypanosomiasis, is transmitted to animals or humans through contact with urine/feces of insect vectors. The most common Chagas vector is the triatomine bug, also known as ‘kissing bug’ [1,2]. Habitats for the triatomine bugs are generally cracks or crevices in poorly-constructed buildings, found in both urban and rural areas [1]. The blood-sucking triatomine bugs feed off of humans and animals – particularly at night. After puncturing the host’s skin for their meal, the bug defecates close by, leaving opportunity for the parasites in the feces to enter the human body [1,3]. However, for the transmission to be successful, the process must be further propagated through human action – such as when a person accidentally or instinctively, scratches the bug’s feces into the skin break, in response to the bite [1].
Chagas: Signs and Symptoms
Chagas disease is clinically identified as occurring in two phases: acute and chronic [4]. The acute phase occurs immediately after infection and can last up to two months [4]. During this phase, the parasitic level circulating in an individual’s blood is high, but symptoms are often mild or asymptomatic [1,4]. In less than 50% of cases, symptoms and signs of infected individuals include fever, headache, pallor, muscle pain, enlarged lymph glands, breathing difficulties, abdominal or chest pain, or swelling [1]. During the chronic phase, parasitic levels decrease, and most infected individuals will enter a “chronic indeterminate” phase, which is a “prolonged asymptomatic form of the disease” [1,4]. The parasites often hide in the heart and digestive muscles during this time [1]. Consequently, some individuals may never develop Chagas-related symptoms, leaving them to be asymptomatic for life. However, up to 30% of infected individuals will develop cardiac disorders, with an additional 10% developing digestive, neurological, or other mixed presentations as a result of their chronic stage infection [1, 4].
Chagas: Treatment and Prevention
Treatment of Chagas disease includes use of medications like benznidazole and nifurtimox, which kills the parasite [1]. These medications are 100% effective if given soon after infection, within the acute phase [1]. The longer an individual is infected, the less effective the medications are in successfully treating the individual [1]. There is no vaccine for Chagas disease [1].
Prevention of Chagas disease is often conducted through vector control techniques, including spraying of houses and surrounding areas with residual insecticides, utilization of bed nets, building improvements to prevent vector infestation, proper hygiene practices in food preparation, consumption, storage, and transportation, as well as screening of blood donors [1]. The screening of blood donors is done to ensure prevention of infection through transfusion and organ transplantation [1].
It’s the Guinea Pig Feasts
Researchers believe that increases in prevalence in certain locations could potentially occur if an increased number of infectious vectors came in close contact with a host population [5,6]. It was concluded in the recent study published in Proceedings of the Royal Society B, that guinea pigs may act as reservoirs of T. cruzi and for the city of Arequipa, Peru, this turned out to be bad news [5,6].
Guinea pigs are commonly raised as food in Peru. Because they can act as reservoirs of T. cruzi, the increased consumption of guinea pigs by humans may consequently increase successful transmission – but not in the way one may think [5,6]. Because guinea pig populations can be fairly predictable – the cost of alfalfa rises during the dry summer months and the guinea pigs that are fed by it are often killed for human consumption. All guinea pigs could carry T. cruzi, but the seasonal culling could leave behind a smaller population for vectors to feed from [5,6]. This results in a higher likelihood of a T. cruzi bug biting into an infected guinea pig, as opposed to a healthy one, and then passing it onto future meals, such as humans [5,6]. The condensing, annual cycle of guinea pig farming could be increasing T. cruzi rates among guinea pigs, Triatomine bugs, and subsequently, humans. According to researchers, this is what’s exactly happening in Arequipa, Peru.
—
Sources
[1] http://www.who.int/mediacentre/factsheets/fs340/en/
[2] http://www.cdc.gov/parasites/chagas/
[3] http://www.cdc.gov/parasites/chagas/epi.html
[4] http://www.cdc.gov/parasites/chagas/disease.html
[5] http://rspb.royalsocietypublishing.org/content/282/1810/20142807