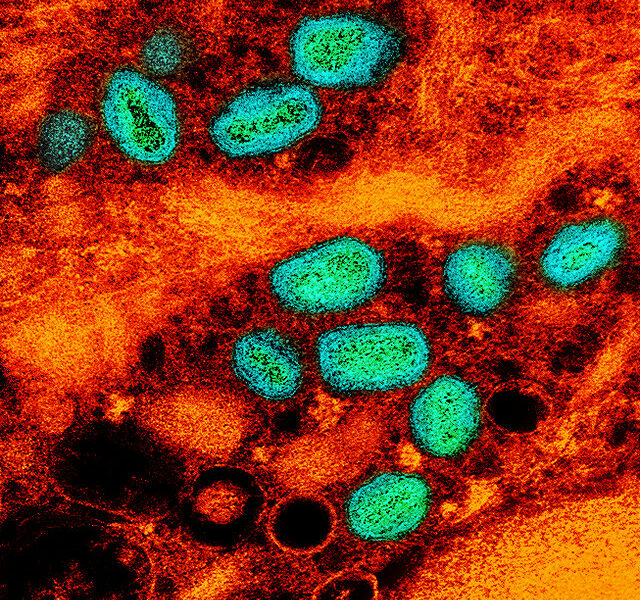
India’s southern state of Kerala was put under a lot of stress this past May with the most recent Nipah virus outbreak. The Nipah virus, which is carried by Pteropus fruit bats, is a newly emerging zoonotic disease that affects both animals and humans. This is the first ever outbreak of Nipah in the state of Kerala [2]. Earlier cases of the virus were reported in West Bengal’s districts of Siliguri in 2001 and Nadia in 2007, with around 47 deaths reported. The first victims of the current outbreak are said to be siblings Mohammad Sadik (26 years old) and Mohammad Salih (28 years old) who died on May 5th and 18th respectively, in Perambra village in the district of Kozhikode [4]. Their aunt and father died a few days after them, along with a nurse that was treating Salih in Taluk Hospital [5]. In late May, Kerala’s state government issued a warning for travelers to avoid the districts of Kozhikode, Malappuram, Waynad and Kannur, as the death count rose to ten [4].
There have been 17 total cases of death from Nipah with one confirmed case recovered [3], but no new cases have been reported since the end of May [2]. Unfortunately, the fatality rate of this outbreak was 70% [3]. Thankfully, the outbreak has been contained, with cases reported now only in the districts of Kozhikode and Malappuram. Not all infected patients seemed to transmit the disease, only those in the acute stages [6], which has helped to avoid a second wave of the outbreak. All known cases thus far were people in contact with the infected brother Salih or who shared a hospital ward with him or with those who became infected. Furthermore, health authorities have drawn up a list of 1,949 people who have been in contact with Nipah-affected people to monitor their health conditions [2].
After the first two victims’ deaths, authorities discovered insectivorous bats living in the well of the infected family, which was their main source of water, but the bats along with local cattle and pigs tested negative for Nipah in Kozhikode [4]. However, authorities tested the wrong kind of bat; fruit bats of the Pteropodidae family, and Pteropus genus are known as the reservoir species for Nipah, acting as the primary host for the virus and carry and transmit it without showing symptoms [6]. This led to confusion and misleading news reports claiming that bats have been proven not to be the source of infection [5]. The government then announced that a multi-disciplinary team was investigating the situation and advised the public not to spread fear and rumors through social media [4].
Even after 21 fruit bat samples tested negative for Nipah, authorities concluded this did not eliminate fruit bats as the source of infection. Nipah outbreaks are very rare because, although fruit bats are common in India, only a few of them are infected with the virus at any one point in time, and they only have a very short window of opportunity to infect others or transmit the virus to humans [6]. Therefore, if a large number of fruit bats is sampled and all of them test negative for Nipah, it does not rule out the bats as the source of infection. Bats may only be infectious for a couple of weeks and then no longer carry the virus. For example, a 2012 study found Nipah in only one of 140 bats tested in Maharshtra and West Bengal and the other bats did not even show evidence of an antibody against the virus [6].
In response to the Nipah outbreak and fruit bat testing, the United Arab Emirates banned imports from Kerala due to fear of spreading the virus through contaminated fruits and vegetables [2]. Fruits and vegetables can become contaminated with Nipah if an infected bat tries to consume fruit or leaves saliva or excretions on it. The virus can then be transmitted to humans or animals who eat any part of the fruit or its juice; furthermore, if an intermediate animal eats contaminated fruit it can also transmit the virus to humans through its saliva and feces. As a precaution, the Kerala state government advised people against eating marked and bruised fruit or fruit found on the ground, to stay clear of areas with bats [2], and to boil drinking water [4].
Although the source of the outbreak in Kerala suggests fruit bats, specifically Pteropus medius [6], the ecological driver and mechanism for the transmission of the Nipah virus is humans. As fruit bats’ habitat is destroyed by humans, they become stressed and hungry, which weakens their immune system, making them more susceptible to the Nipah virus and causing them to excrete the virus through their urine and saliva [4]. For example, the El Nino event in 1997 led to fires in Kalimanatan and Sumatra in Malaysia, destroying approximately five million hectares of forest. The haze from the fires badly affected flowering and fruiting trees in southern Malaysia, forcing fruit bats to migrate to orchard farms surrounded by pig farms, leading to transmission of the virus from bats to pigs to humans. It is important to bring awareness of the impact humans have on bat species and to prevent disproportionate fear and negative sentiment that may lead to animal culling. Fruit bats are an important ecological species for pollination and seed dispersal, preventing deforestation [6].
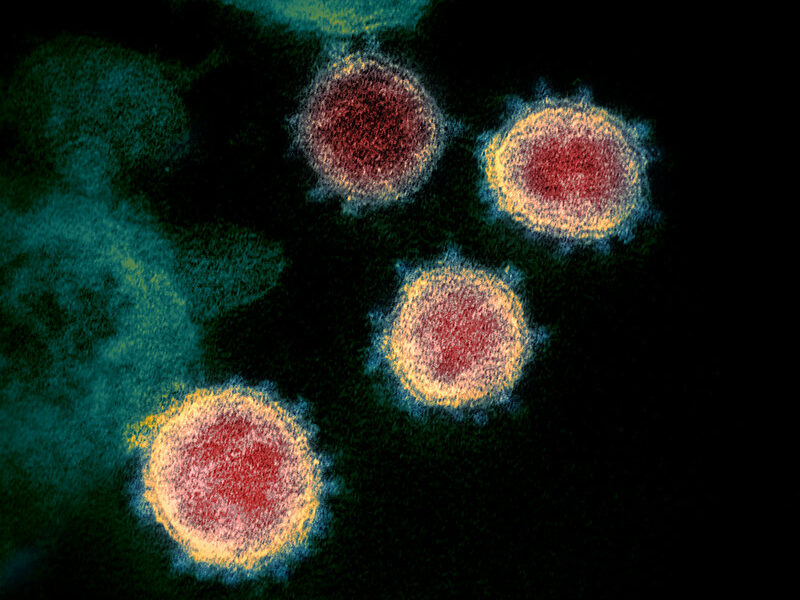
The Nipah virus was first detected as the source of an outbreak in Malaysia in 1998-1999 and was named after the Sungai Nipah village on the banks of the Nipah River [5]. The virus belongs to a genus of paramyxoviruses (Heniparivurs), which includes the Hendra virus found in Australia that causes acute respiratory distress and encephalitis. Previous studies on outbreaks show that Nipah virus can be transmitted to humans in three different ways. The first is from infected bats to humans who come in contact with material contaminated by bats; between 2001 and 2007 in Bangladesh, there were more than 20 incidences of bat to human transmission reported through the consumption of date palm sap contaminated by bat urine or saliva [6]. This is the most likely route of transmission in the current outbreak as the palm sap is commonly used in Indian drinks [4]. A second way is from intermediate hosts such as pigs, horses and other domesticated animals; the outbreak in Malaysia in 1998 was traced from pigs who ate fruits infected by bats and then passed it to humans [6]. The last route of transmission is from infected humans. Risk of transmission between humans is relatively low because it requires close contact with bodily secretions such as urine and saliva [5].
Ways of preventing transmission include: actively monitoring and quarantining suspected cases; using gloves, masks and face shields to limit spread; funeral practices that avoid bodily fluids; and reduction of fomite transmission by cleaning surfaces in contact with infected people [5]. The incubation period ranges from four to 14 days, leading to clinical symptoms that include fever and headaches, which can progress to drowsiness, disorientation, mental confusion, and encephalitis in less than a week. There are no drugs or vaccines to treat Nipah, intensive supportive care is the only recommended treatment [4]. However, the Indian Council for Medical Research (ICMR) reached out to the University of Queensland, Australia in May to develop an antibody [2], which it arrived in Kozhikode on Saturday June 2nd and was administered to cases who tested positive that following week [1]. The antibody does not act as a vaccine, but acts to neutralize the effects of the virus. In terms of detecting Nipah infection, molecular tests such as polymerase chain reaction (RT-PCR) and next generation sequencing are the most rapid and accurate tools available, using body fluids such as blood and saliva [5]. Additionally, an enzyme-linked immunosorbent assay (ELISA) test can detect the entire viral antigen.
Sources:
[1] “Antibody to Fight Nipah Reaches Kozhikode.” The Hindu, The Hindu, 2 June 2018, www.thehindu.com/news/national/kerala/antibody-to-fight-nipah-reaches-kozhikode/article24069637.ece
[2] “As Kerala Health Officials Warn of Second Nipah Virus Outbreak, Here's All You Need to Know of the Infection.” Firstpost, Firstpost, 2 June 2018, www.firstpost.com/india/as-kerala-health-officials-warn-of-second-nipah-virus-outbreak-heres-all-you-need-to-know-of-the-infection-4492509.html
[3] Gulland, Anne. “Nipah Outbreak: India State on Alert after Bat-Borne Virus Kills Three.” The Telegraph, Telegraph Media Group, 12 June 2018, www.telegraph.co.uk/news/2018/06/12/nipah-virus-control-india-britain-world-must-alert-signs-infected/
[4] John, Haritha, and Gopikrishna Warrier. “Nipah Infection in Kerala: Don't Blame the Bats Alone; Improve Public Health.” Mongabay-India, 30 May 2018, india.mongabay.com/2018/05/30/nipah-infection-in-kerala-dont-blame-the-bats-alone-improve-public-health/
[5] Lee, Benhur, and Linfa Wang. “Update on the Nipah Virus Outbreak in Kerala, India.” GVN, Communications, 30 May 2018, gvn.org/update-on-the-nipah-virus-outbreak-in-kerala-india/
[6] Rao, Nithyanand. “The Absence of Evidence for Nipah in Fruit Bats Is Not Evidence of Absence.” The Wire, The Wire, 30 May 2018, thewire.in/health/the-absence-of-evidence-for-nipah-in-fruit-bats-is-not-evidence-of-absence